European public healthcare is facing a critical moment. In countries like Spain and France, longer life expectancy and the prevalence of chronic diseases have placed unprecedented pressure on health systems. In Spain, the Madrid region recorded a total of 1,029,742 medical appointments on the waiting list in August 2024, marking a historical record. According to the July 2025 Health Barometer by CIS, 24 percent of the population waits more than eleven days to see their general practitioner, and the average waiting time for a specialist reaches 115 days. In France, while healthcare coverage is universal, inequalities and growing reliance on complementary private insurance make rapid access to certain services increasingly dependent on patients’ financial capacity. These data indicate that the problem is not temporary or solely post-COVID, but structural, combining staff shortages, service pressure, and demographic challenges affecting both countries.
Healthcare Systems and Main Challenges
The Spanish National Health System is universal and tax-funded, with primary care playing a central role. Despite its historical strength, resources are currently insufficient to meet demand. Each doctor performs an average of 6,906 consultations per year and each nurse around 4,104, reflecting the daily workload pressure. Unequal geographical distribution of professionals and limited training capacity hinder staff replacement, particularly in rural areas.
In France, the healthcare system combines public hospitals and private providers under a social insurance model. In cities such as Paris, hospital capacity is high, but pressure on healthcare professionals is significant. The average number of doctors is 4 per 1,000 inhabitants and nurses 9 per 1,000, but staff shortages result in long shifts, high stress, and increasing burnout risk. Per capita spending is higher than in many European countries; however, system organization and staff management, not only funding, determine efficiency and sustainability.
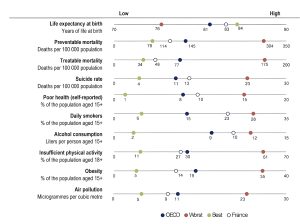
Comparing key health indicators helps illustrate the challenges each system faces, from life expectancy to lifestyle-related risks.
Staff Shortages and Consequences
The lack of healthcare professionals is a Europe-wide phenomenon. It is estimated that the shortage could reach 4 million workers by 2030 if no measures are implemented. This directly affects patients, who face long waiting lists, overcrowded primary care centers, and pressure on emergency departments. For professionals, the situation leads to burnout, emotional exhaustion, and ethical frustration. A joint study by CSIC and the Carlos III Health Institute indicates that one in six primary care workers suffered from burnout, affecting 25 percent of doctors and 16.7 percent of nurses.
Recent protests by healthcare workers in Spain during 2024 and 2025 highlighted concerns over workload, low salaries, and lack of professional recognition. Thousands of doctors, nurses, and assistants demonstrated in several cities, demanding improvements in working conditions and increased investment in primary care. In France, similar protests were reported, particularly among emergency staff and nurses in Paris, calling for more personnel and better hospital conditions. These mobilizations reveal the social and political dimension of the healthcare crisis, as professionals advocate for both their wellbeing and the quality of patient care.
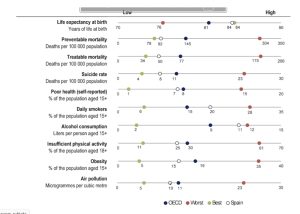
A closer look at Spain shows how structural pressures translate into health outcomes for its population.
Impact on Patients and Inequality in Access
The healthcare crisis has tangible effects on patients. In Spain, overloaded primary care and long waiting lists for specialists and diagnostic tests can delay diagnoses and worsen health outcomes. In France, although access is relatively quick in major cities, reliance on complementary insurance creates inequality, making rapid access dependent on financial means rather than medical need. The growth of the private healthcare sector in Spain, which reached €13.9 billion in 2023 and performed nearly half of hospital procedures and more than a third of emergency visits, shows that patients are seeking alternatives due to delays in the public system.
Institutional Responses and Innovations
Both countries have implemented measures to improve efficiency and reduce pressure. Telephone appointments and telemedicine allow urgent cases to be prioritized and waiting times to be reduced. Shift reorganization and flexible schedules aim to balance the workload of staff. Digital medical records and appointment systems reduce administrative burdens, freeing professionals to focus on patient care.
Training programs and incentives aim to retain doctors and nurses in the public system, while psychological and ethical support provides guidance for handling professional dilemmas and stress. While these measures are helpful, experts stress that structural reforms are necessary to ensure sustainability and long-term workforce wellbeing.
Voices from Healthcare Professionals
The accompanying audio report takes listeners inside hospitals and health centers in Spain and France, capturing the daily realities of the healthcare system. In it, you will hear the experiences of doctors, nurses, and patients as they navigate long working hours, high patient loads, and the challenges of providing care under pressure. The recordings highlight both the human impact of staff shortages and the practical solutions being tried, from teleconsultations to reorganized schedules
Towards Sustainable Solutions
Telemedicine, shift reorganization, digitalization, and psychological support are first steps, but long-term sustainability requires a comprehensive approach, including workforce planning, improved working conditions, and strategic public investment. The experiences of Spain and France show that high spending alone does not guarantee optimal outcomes or equity. Efficient staff management and system organization are key to maintaining strong, sustainable public healthcare systems. slot88 resmi
The healthcare systems in Spain and France face a structural challenge that goes beyond temporary crises. Staff shortages, long waiting lists, and unequal access highlight the urgent need for systemic reforms. Measures such as telemedicine, flexible shifts, and digitalization are important first steps, but long-term sustainability will require strategic investment, better workforce planning, and improved working conditions. Ensuring that public healthcare remains universal, efficient, and resilient depends on balancing the needs of patients with the wellbeing of the professionals who care for them, making human resources the cornerstone of a sustainable system.




