Side-effects of hormonal contraceptives, including the oral contraceptive pill, the Intrauterine Device (IUD) and the implant, are common. One in ten women experiences mood swings, headaches, a decreased sexual libido, weight gain, acne and a different stress reaction, according to the prescription provided with the contraceptives. Doctor Lilian van Raalte sees this reflected in the consults made in her doctor’s office. “Many women feel they experience these consequences of their contraceptive use,” she says.
Though a lot of research has been done to expose the physical health effects of pill use – since the pill is older and more known than the IUD and implant –, not a lot is known about the mental health effects. Worldwide, 151 million women use the pill. In 2016, Danish researcher Charlotte Skovlund completed a study about depression and the contraceptive pill amongst one million Danish women. She concluded that a correlation was evident: a greater number of women taking the pill also experienced depressed feelings, especially amongst adolescents. However, it was not studied whether depression caused pill use, or vice versa. Sometimes when a woman is depressed, a contraceptive pill is prescribed to calm the hormones and stabilise the mood. This effect is different on everyone.
“The psychological effects of the contraceptive pill are highly understudied. Something we are just now learning more about is the impact it has on mood,” says assistant professor Estrella Montoya of Utrecht University, who has written her dissertation on the effects of contraceptive hormones on the body. “The pill can cause both negative and positive feelings, leading to depressed feelings on the one hand, or an increased positive feeling on the other hand. It differs per user, but this effect occurs amongst one in ten women,” she says. Other effects are an alteration in feelings of attraction, stress, emotion regulation, friendships and changed hunger patterns, says Montoya.
67% of women between ages 15 and 49 use contraceptives, over half of which use the oral contraceptive pill. In the past years, many women have switched to the Intrauterine Device (IUD). This long-acting birth control method is impossible to forget, since it is placed in the uterus and doesn’t need to be swallowed daily like the pill. It is less expensive and excretes less hormones than the standard contraceptive pill. However, placement is painful and cysts can occur. And though there are less hormones excreted, the hormones still impact the way the woman is feeling, says Montoya.
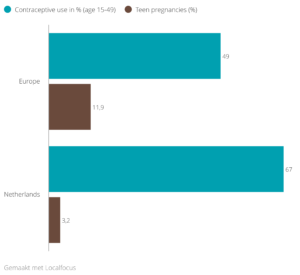
Figure 1. Percentage of contraceptive use and teen pregnancies in the Netherlands and Europe, 2017
Student Camille van den Boorn (24) was a mere twelve years old when doctors prescribed her a contraceptive pill due to heavy menstrual bleeding. Recently, she began to question what effect these synthetic hormones had on her mental well-being, as she had suffered through turbulent puberty years including a depression. At 24, she quit using the pill, and noticed she feels better. “I have stopped having migraines around my menstruation. I don’t feel bloated anymore. And I am now able to distinguish where my emotions come from, and how I can deal with them,” says Van den Boorn. “Around me, I heard more and more women starting to question the pill, and I was wondering to what extent it was impacting me. The annoying thing is that you don’t know what the effect it until you have stopped using it,” she says.
Montoya has also researched what the pill does to the stress reaction. “Normally we produce cortisol, a hormone that enables us to deal with stressful situations. But we see that this cortisol production is lower amongst women who take the pill,” the psychologist says. She states that this lowered stress reaction is also something which is evident amongst people with a depression. However, a difference is found with the IUD, which only excretes progesterone. “Progesterone-only birth control methods actually increases cortisol production, leading to an increased reaction to stress,” says Montoya.
Also, Contraceptive pills can decrease the level of testosterone by 70% in the female body. “Testosterone is extremely important for sexual libido and mood,” says Montoya. Now new contraceptive pills are being developed which include testosterone, to fill in the shortage.
Only recently have mental side-effects received more attention. In the summer of 2020, the Dutch Doctor Society (NHG) altered the guidelines for the prescription of contraceptives, so that psychological side-effects are included in the information given to women wanting to start using them. Ineke van der Vlugt is programme leader at the Dutch Knowledge Centre of Sexual Health Rutgers. She says: “Psychological wellbeing is considered more important now. Previously, most attention had been given to the effect of the pill on for example thrombosis or cancer, but not on the mental wellbeing.” Montoya agrees with this: “Psychological effects are seen as secondary effects. There is a significant knowledge gap between physical effects and psychological effects.”
Link to interactive infographic: https://localfocuswidgets.net/5ff86f83b4689
Some people disagree with the recent augment in careful attention being paid to the effect of hormones on the body. Gynaecologist Jelle Stekelenburg, professor at Groningen University in the north of the Netherlands, compares it to “a hype” that women are “tired of hormones”. Stekelenburg says: “The hormones used in the pill and the IUD are very similar to the hormones present in the female body.” A lot of women come to his office and state they don’t want to take any more hormones. Stekelenburg: “I’m afraid many women blame differing complaints on their hormonal cycle, though there isn’t always sufficient ground for that.”
The lack of concrete knowledge and evidence is something women are struggling with. Van den Boorn sees women around her hesitant in stopping their pill intake. “They are wondering what the effect is on their body. But the downpart is that stopping means you need to find a different way to protect yourself against pregnancy,” she says.
Is the awareness about the effects of hormonal birth control a recent phenomenon? Stekelenburg thinks back to the 1960s, when the pill was celebrated as the emancipation of females. “Women had fought for decades for contraceptives. Now it almost seems as if hormones oppressing women,” he says.
In society, Van der Vlugt witnesses a collective aim to be a perfect, most natural version of oneself. “Especially amongst higher educated women, a wish to be ‘pure’ is popular. Synthetic hormones don’t fit into this image of natural perfection,” she says. Stekelenburg agrees. “It is no longer all right to feel bad anymore. One must be pretty, social and always have enough energy to do sports. But sometimes, this just isn’t the case. Whether you do or don’t take hormones,” he says.
American psychologist Sarah Hill, known for her book This Is Your Brain on Birth Control: The Surprising Science of Women, Hormones and the Law of Unintended Consequences (2019), was one of the first to openly address the consequences of hormones crossing the membrane barrier into the brain. “This means women are a different version of themselves when they are on birth control,” the psychologist writes in her book. The idea that IUDs only excrete hormones affecting the uterus, is a myth, says Montoya. “Hormones enter your blood. It’s not just your uterus, not just your brain: it’s your whole body that is affected,” says Montoya. However, little research has been done about the psychological effect of an IUD.
Steps can be taken to increase awareness for the psychological effects when girls and women speak to their doctors, right before starting birth control. “Research I am conducting now is showing many women want more information about mental consequences when starting hormonal birth control,” says Montoya. She feels doctors should be clear about these consequences, especially about the impact on mood. Doctor Van Raalte sees the benefit in this also, though she notes that time is scarce in doctors’ offices. “Women should be more aware of the side-effects of these medicine. If you are doubting what effect it has on you, stop for two months and examine carefully how you feel,” says van Raalte.
Montoya has a clear view on it. “Doctors ought to call back the women two months after starting contraception, to check how it is going. Hormonal changes are very drastic, and this is something that should be communicated well,” she says.




